The Hills
Addiction
Treatment Programme
At The Hills, your safety and well-being are our top priorities. We know that addiction is a deeply personal struggle, and no two journeys are the same. That’s why we believe that recovery is about more than just overcoming addiction—it’s about restoring balance, building resilience, and rediscovering the joy in life. Our daily and weekly routines are thoughtfully designed to support your physical, emotional, and spiritual well-being.
To ensure you’re fully supported, our substance abuse treatment programmes include a carefully customized detox process tailored to meet your unique needs. This approach ensures that you go through detox in the safest and most comfortable environment possible, with expert medical supervision and care.
Our Commitment

Personalized Care with a Fully Licensed Psychiatrist
From the moment you arrive, our fully licensed psychiatrist will work closely with you to create a treatment plan that fits your specific needs. Whether you’re facing mental health challenges alongside substance abuse or require a particular therapeutic approach, our psychiatrist is here to guide you every step of the way.
24-Hour Nursing Staff for Continuous Support
Our 24-hour nursing staff provides constant care and support. They’re always available to help with any concerns, ensuring that you feel safe and looked after at all times.


On-Site Hospital for Immediate Medical Attention
In addition to our expert care team, we have an on-site hospital ready to handle any medical needs that may arise. This ensures that you receive immediate attention if necessary, making your recovery process as safe and smooth as possible.
Tailored
Detox
Process
Detoxing can be one of the hardest parts of recovery, but you won’t have to go through it alone. Our detox process is customized to your specific situation, helping you through withdrawal in a comfortable, controlled environment. With medical supervision and support from our staff, we’ll make sure you’re ready to move forward in your recovery journey.
Alcohol Detox
Get the help you need to safely stop drinking, with a detox plan that fits your situation.

Drug Detox
Get the help you need to safely stop drinking, with a detox plan that fits your situation.

Prescription Drug Detox
Get the help you need to safely stop drinking, with a detox plan that fits your situation.

Daily Routine
Once detox is complete, the next crucial step is to establish a healthy and structured routine that not only supports your sobriety but also helps you address and overcome the addictive behaviors that may have developed over time. This is where our comprehensive daily routine comes into play.
At The Hills, every part of your day is designed to help you not only break free from addiction but also to confront and change the behaviors that fueled your substance abuse. Our structured routine supports your physical, mental, and emotional recovery, providing you with the tools you need to rebuild your life and maintain lasting sobriety.
Research has shown that having a daily routine can significantly aid in recovery from substance use disorders. For instance, studies have found that structured schedules can improve emotional stability and reduce cravings, ultimately contributing to better outcomes in addiction treatment . For more information, you can explore studies on the impact of daily routines in recovery here.

- Morning : Start your day with a refreshing off-site walk or jog, followed by mindfulness, breath work, stretching, or meditation. These practices are not just about physical health—they’re crucial in resetting your mind and body, helping you develop healthier habits to replace the routines that might have supported your addiction.

- Mid-Morning : Before lunch, you’ll participate in two group sessions: a Process Group, where you can openly share and reflect on your journey with others who understand what you’re going through, and a CBT or DBT session, depending on the day. These sessions are focused on addressing the root causes of your addiction, helping you develop new coping strategies and break the cycle of addictive thinking.

- Midday: After the group sessions and lunch, Mondays are reserved for Art Therapy or a spiritual chat with a monk, rotating weekly. These sessions help you explore deeper emotional issues and provide a creative or spiritual outlet for the feelings that can often trigger addictive behaviors. On other days, you’ll engage in TRE (Tension & Trauma Releasing Exercises) or Focus Group activities designed to help you release stress and trauma, which are often at the core of addiction.
- Afternoon: Your afternoons also include 1-on-1 sessions like personal training, counseling, and massages, all tailored to your needs. These personalized sessions focus on rebuilding your self-esteem and physical health, both of which are often diminished by addiction. By working on your personal goals, you’re directly confronting and replacing the unhealthy behaviors associated with substance abuse.

- Evening: After dinner, the day concludes with a reflection session, giving you the chance to process what you’ve learned and experienced. This time of reflection is crucial for reinforcing the day’s work, helping you internalize the changes you’re making to your thoughts and behaviors.
Weekly Highlights
- Throughout the week, you’ll participate in specialized group sessions, like AA meetings, Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), or holistic treatments such as Aqua Aerobics. These sessions help you recognize and change the behaviors that drive addiction. Each session is designed to offer you tools to better understand yourself and your habits, providing a clear path to long-term recovery.
Weekend Activities
We understand that transitioning back to normal life is essential in the recovery process. Our weekend activities are tailored to help you apply the new skills and habits you’ve learned throughout the week:
Saturdays: We offer self-care services like haircuts and manicures/pedicures to help you feel your best. Taking care of your appearance is an important part of rebuilding self-esteem during recovery.
Sundays: Our excursions take you outside the center for exposure therapy, where you can practice navigating real-world environments. These trips help ease the transition from the safe rehab space into daily life and allow you to integrate the coping mechanisms you’ve developed throughout your journey.
At The Hills, every part of your day is designed not just to support your recovery here, but to equip you with the tools and routines you need to build a healthier, happier life once you return home.
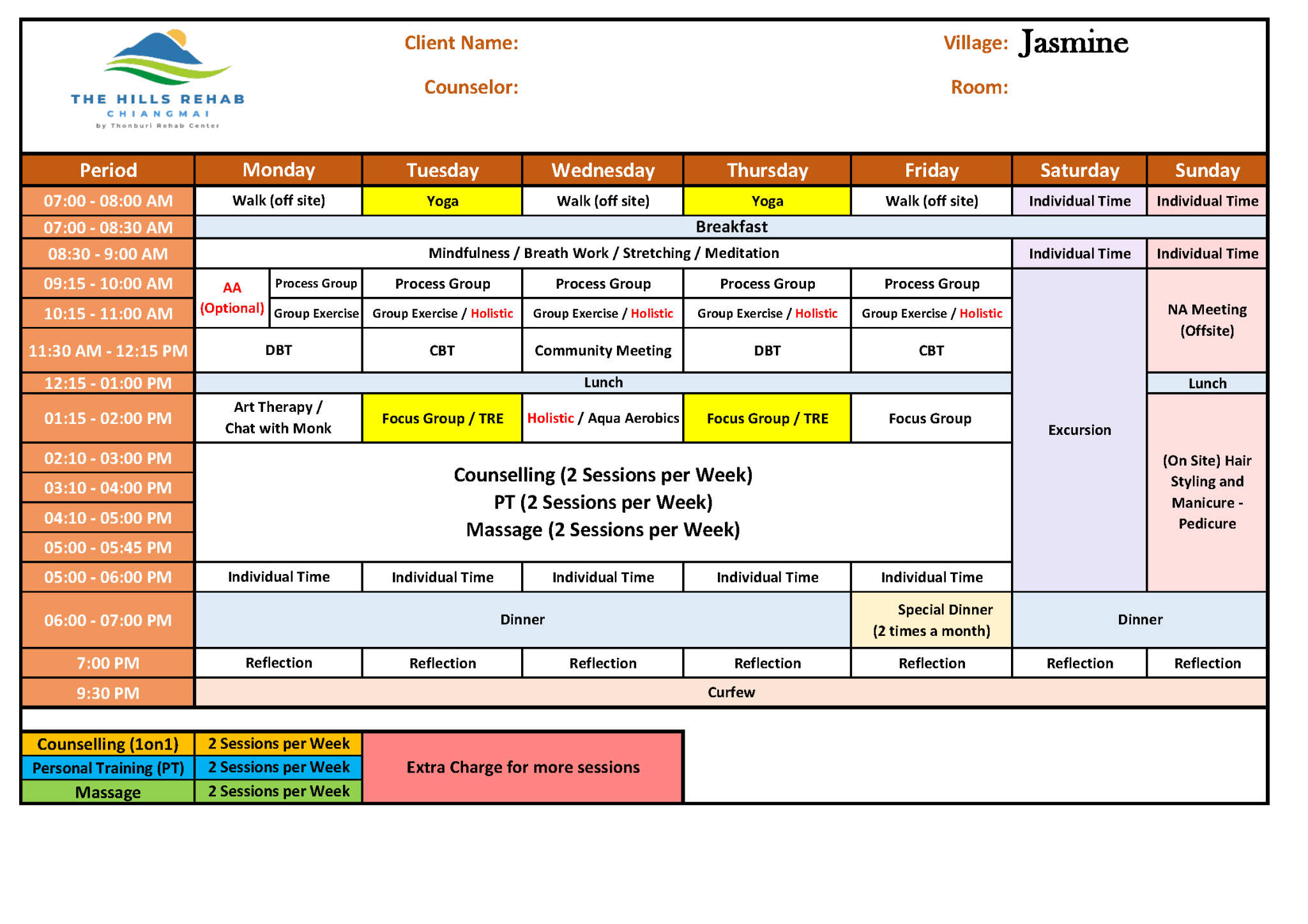
Detailed Schedule Template
To give you a clearer idea of how each day is structured at The Hills, we’ve provided a detailed template of our schedule below.
Take a look at the schedule for a more in-depth look at an example of a real day-to-day routine. If you’d like more information, feel free to contact us.
When to Seek Help
If you’ve been struggling with substance use or feeling overwhelmed by addiction, it’s important to reach out for help. Recognising that you need support is a crucial first step on your journey to recovery. Addiction can be difficult to confront alone, and a mental health professional can collaborate with you to develop a personalised treatment plan that meets your unique needs.
At The Hills, we understand that seeking help is vital for overcoming addiction. Our dedicated team is here to guide you through this process, providing the support you need to reclaim control over your life.

